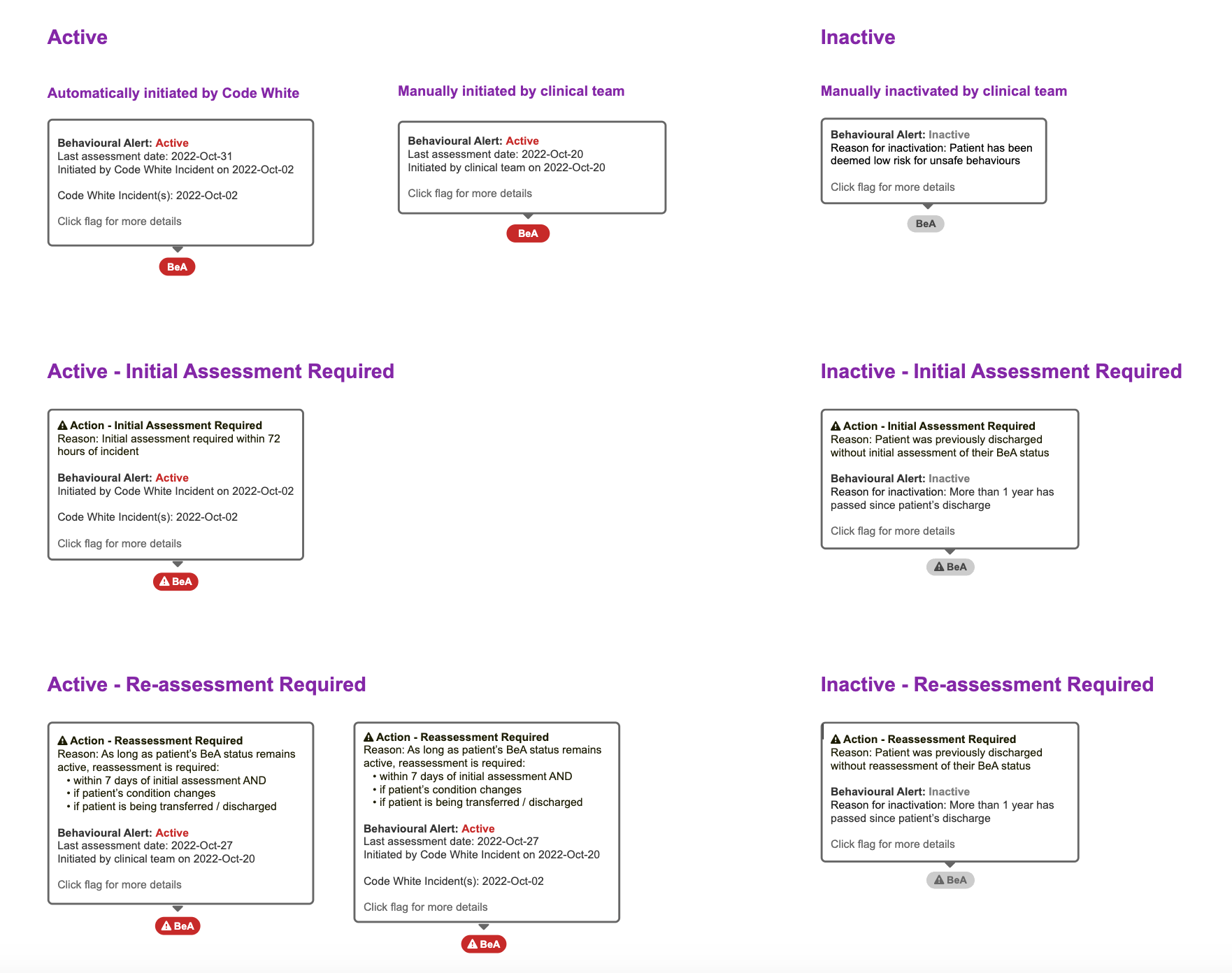
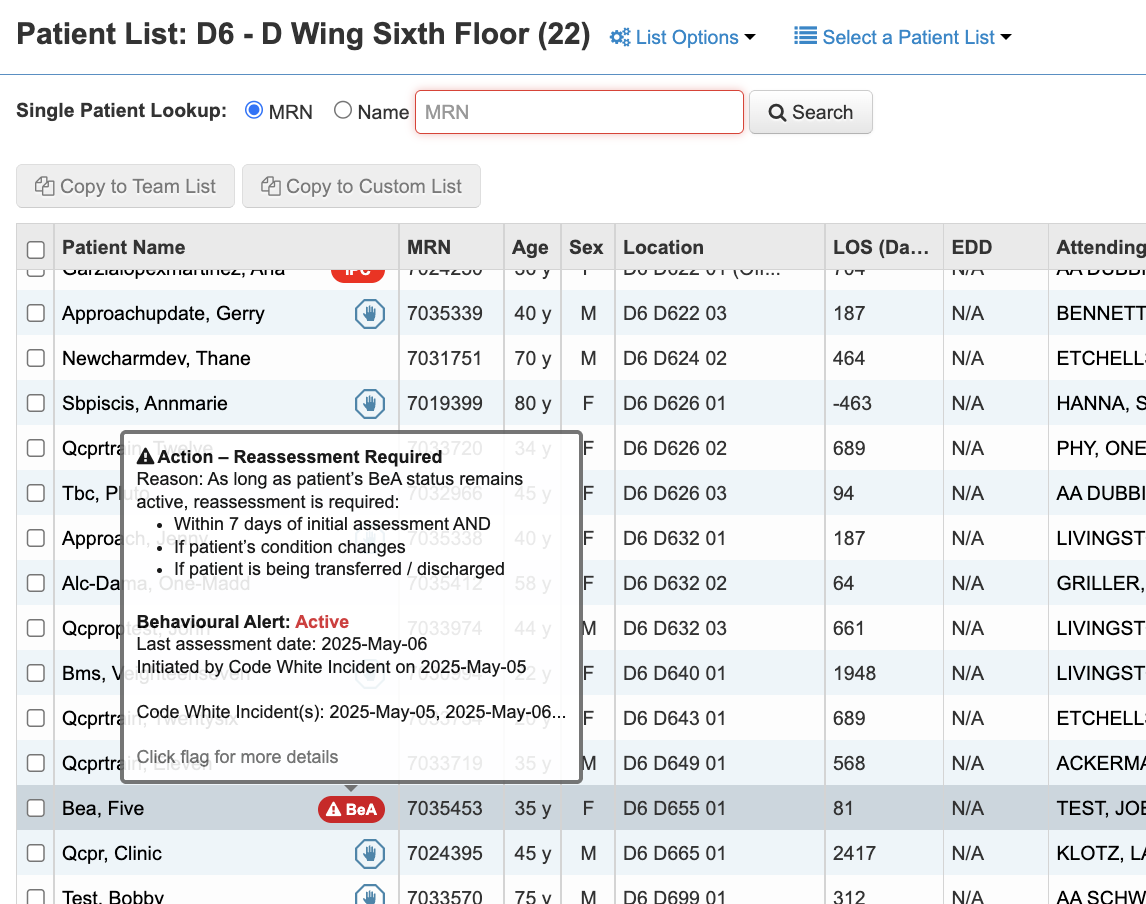
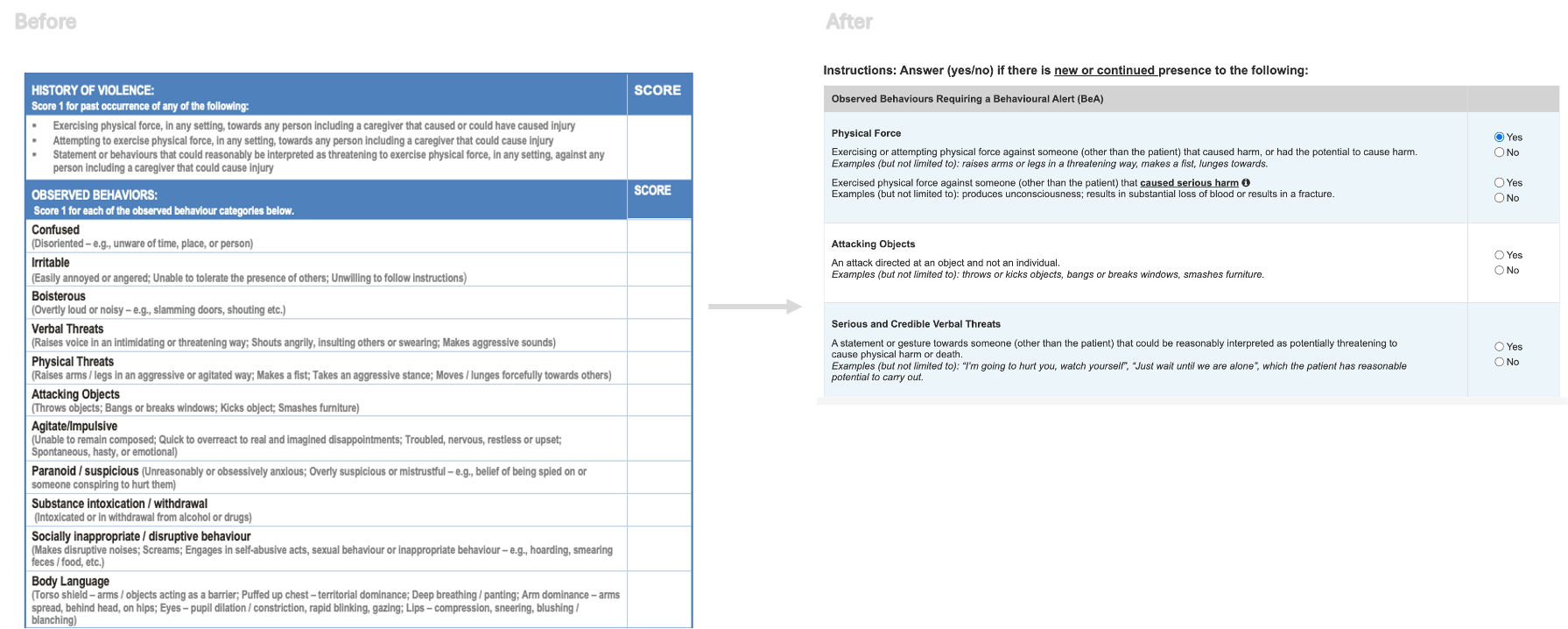
Timeline
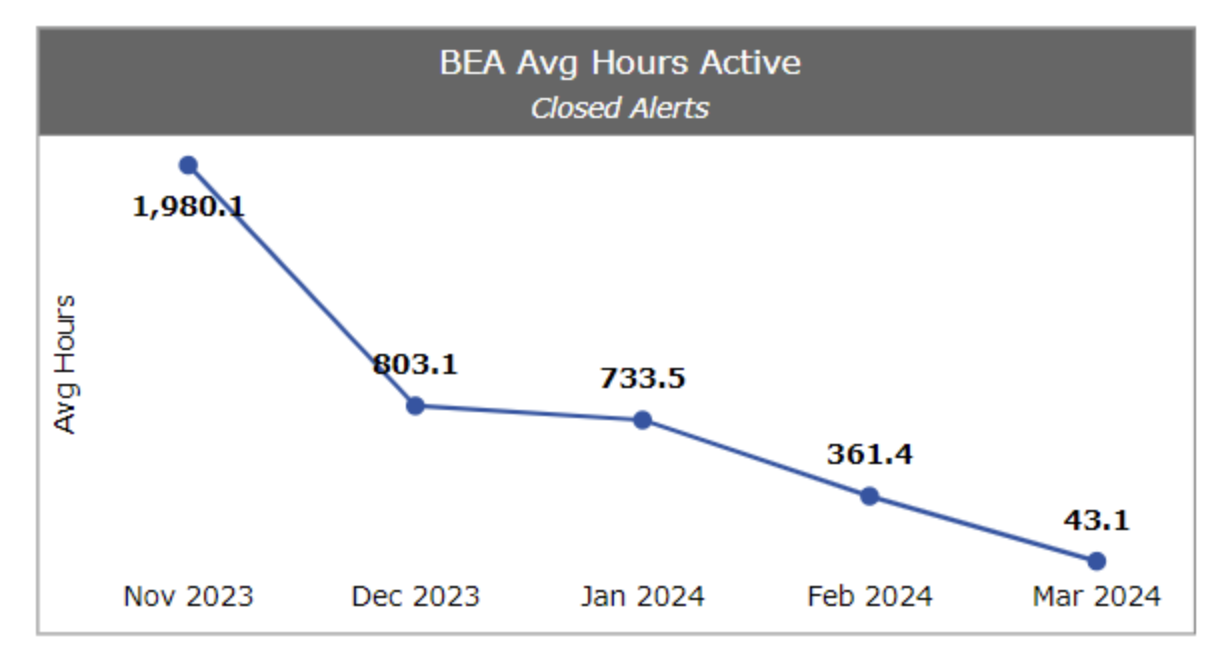
Jan 2022 to Nov 2023
Client
Sunnybrook Health Sciences Centre (SHSC)
Role / Team
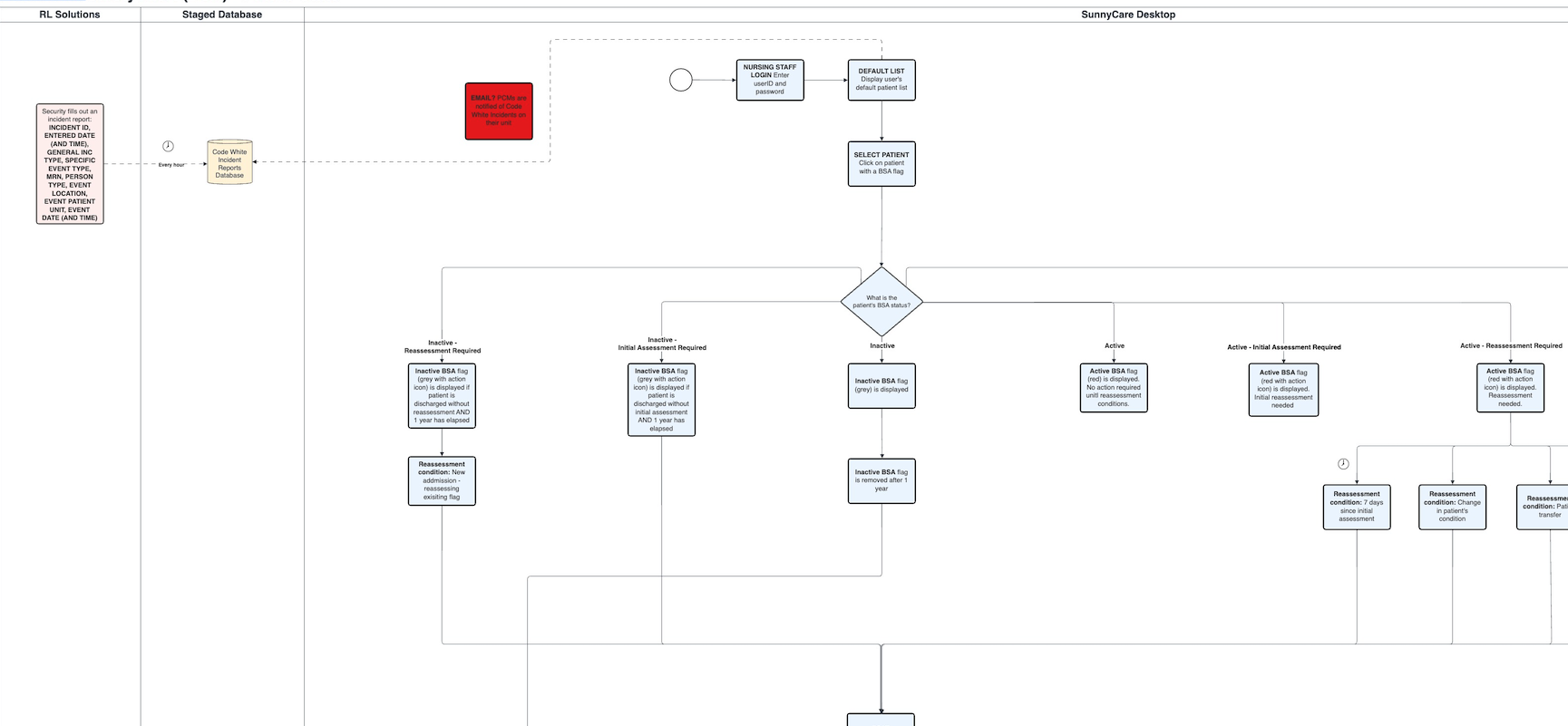
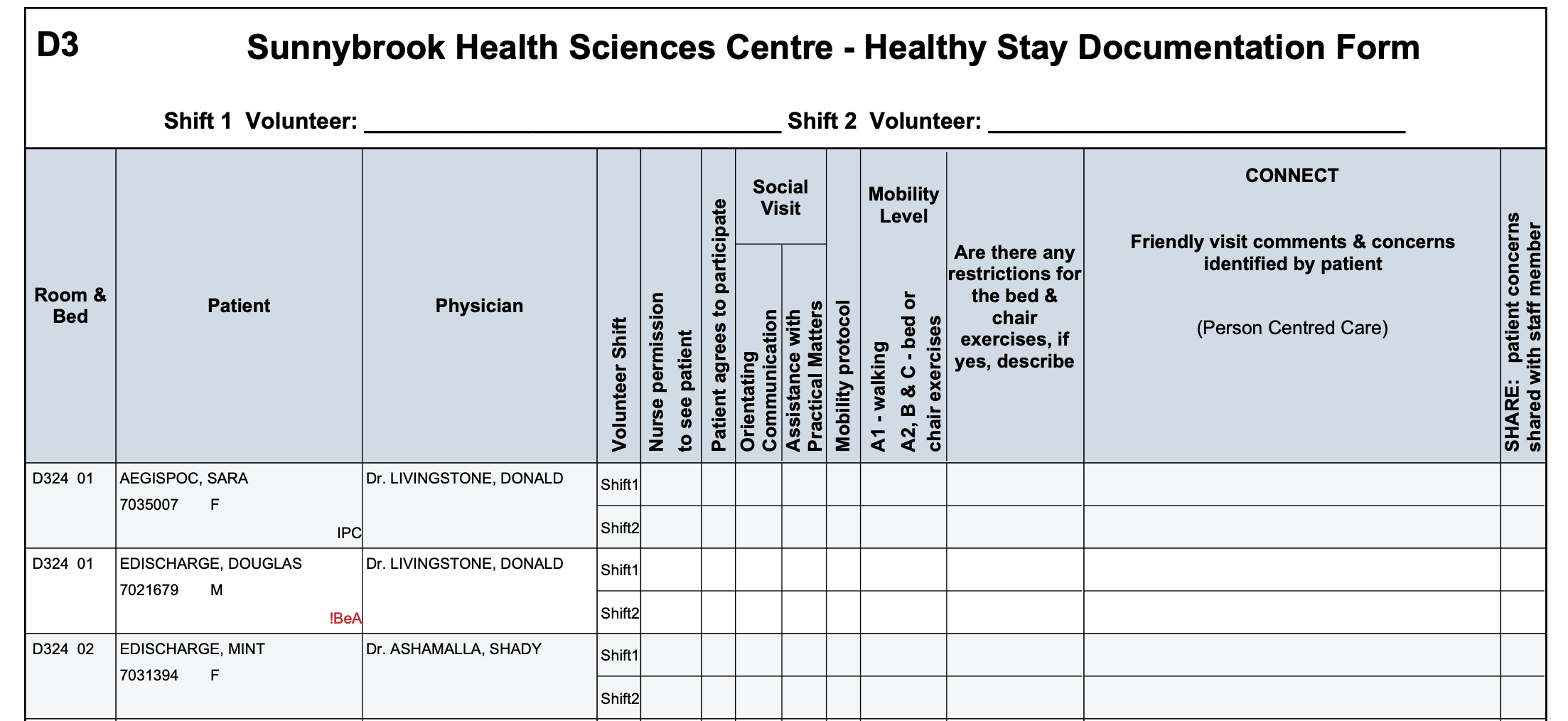
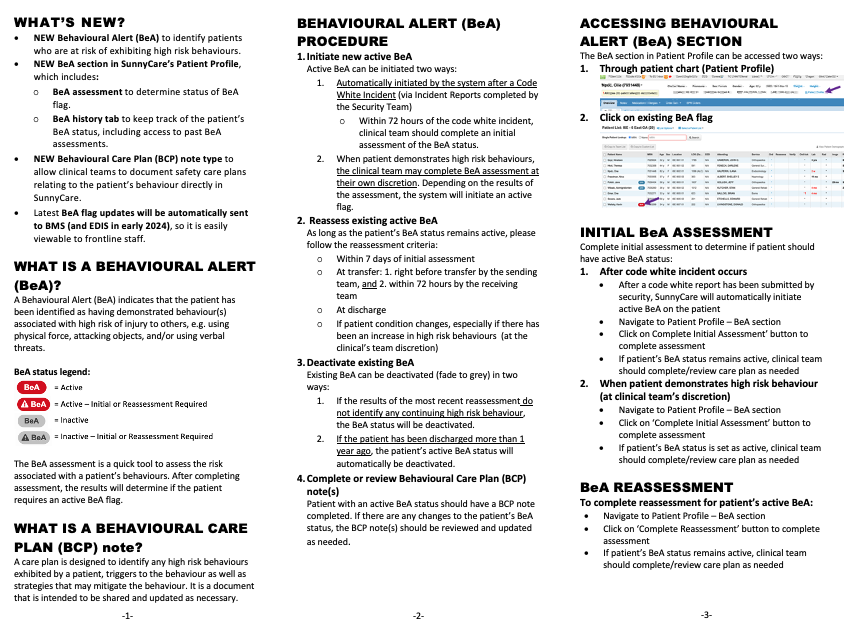
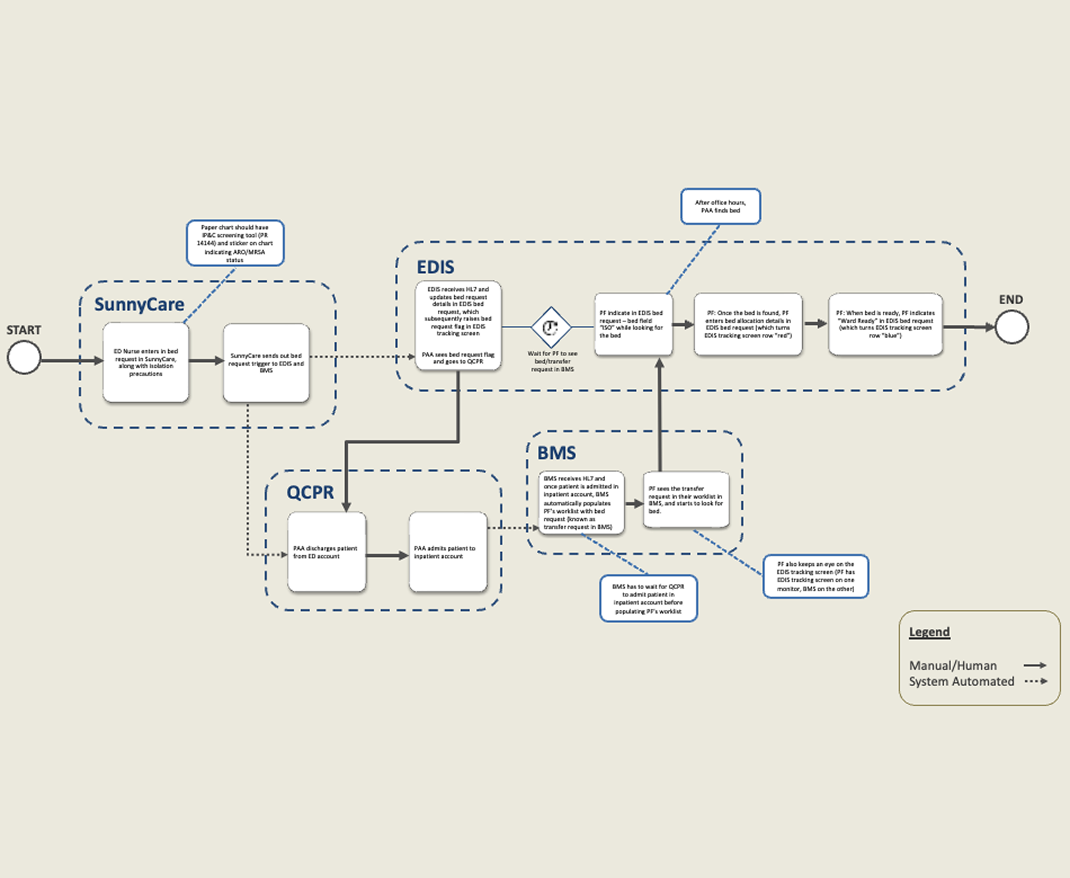
UX Design Specialist and Software Liaison for the Patient Violence Flagging Working Group (PVFWG), along with 2 developers
Platform
Website App
Tools
Axure, Figma, Jira
Methods
Workflow Analysis, Usability Testing (Moderated, In-person and Remote)
.png)