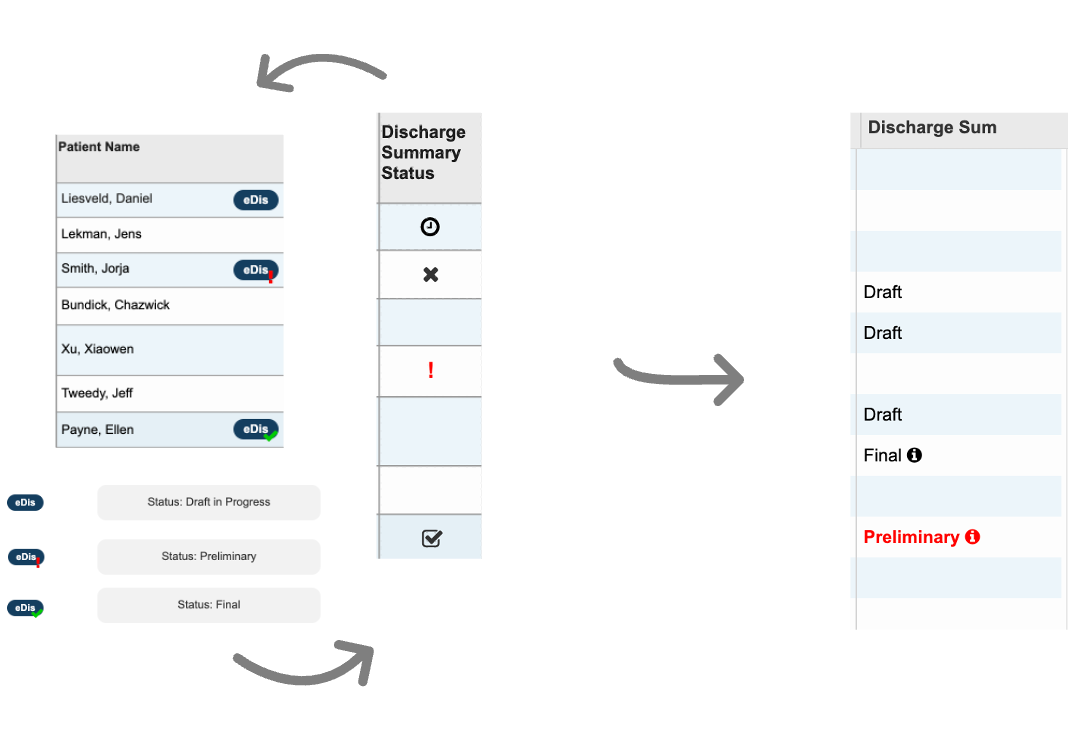
During development, I oversaw QA testing efforts, including testing integration with ancillaries to ensure that discharge summaries are being distributed successfully, and ran data migration test runs on our stage environment. There were also multiple modes of delivery, e.g. manual, auto-fax, electronic, and our team worked to ensure those channels were thoroughly tested.
Test scenarios for HRM and autofax distribution channels

As project lead,
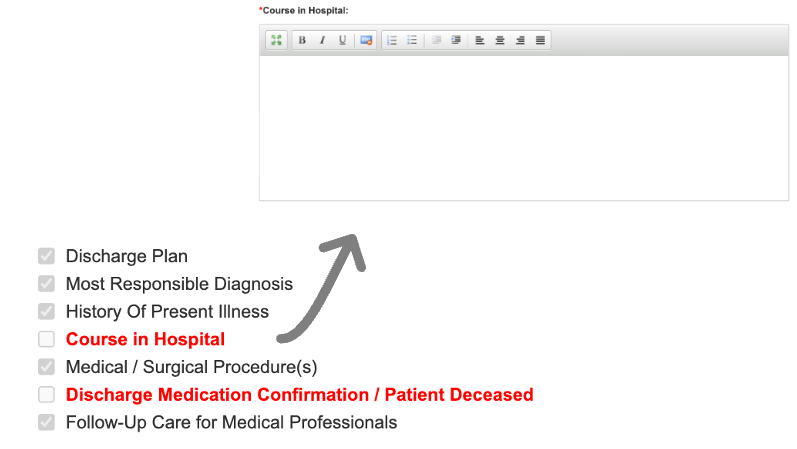
I also led 10 user acceptance test sessions with representative users to ensure that the developed software can handle necessary tasks in real-life scenarios. I took this opportunity to fine-tune the design, e.g. automatically defaulting to the patient’s encounter to save clinicians a click, if the patient only has one encounter.